If a prenatal ultrasound detects spina bifida, the Fetal Center at Riley Children’s Health offers fetal repair to close the birth defect to reduce morbidity and improve health outcomes.
What is Myelomeningocele?
What is Myelomeningocele?
Spina bifida refers to a congenital birth defect in which a baby’s spine does not form properly. Myelomeningocele (also referred to as an “open neural tube” defect) is the most severe form of spina bifida, where the spinal cord and nerves (also known as the “neural placode") develop on the outside of the body. Because of congenital malformations in the spinal cord and nerves, babies can lose function below the spinal level where the neural placode is located. If the neural placode is located higher up on a baby’s back, more nerves have not formed correctly and can result in weakness in the legs, difficulty with walking, and disturbances with bladder and bowel control.
Other commonly encountered forms of spina bifida include spina bifida occulta (the mildest form of spina bifida), meningocele, and lipomyelomeningocele. In these forms of spinal bifida, the spinal cord isn’t on the outside of the body and there is little to no nerve damage.
Medical conditions associated with myelomeningocele
The number and severity of problems in children with myelomeningocele varies depending on where the neural placode is located on the spine and how much of the spinal cord is affected. Possible health effects of myelomeningocele include:
- Hydrocephalus
- Chiari 2 malformation
- Loss of feeling and decreased function or paralysis
- Loss of bowel or bladder control and increased risk for urinary tract infections
- Heart problems
- Orthopedic issues, particularly clubfoot malformations
- Other neurological problems
How is myelomeningocele diagnosed?
Myelomeningocele can be diagnosed early in pregnancy and most commonly during the anatomy ultrasound at routine prenatal visits and prenatal ultrasounds. If diagnosed, mothers may be eligible for fetal surgery to repair the myelomeningocele before birth.
What is Fetal Myelomeningocele Repair?
What is Fetal Myelomeningocele Repair?
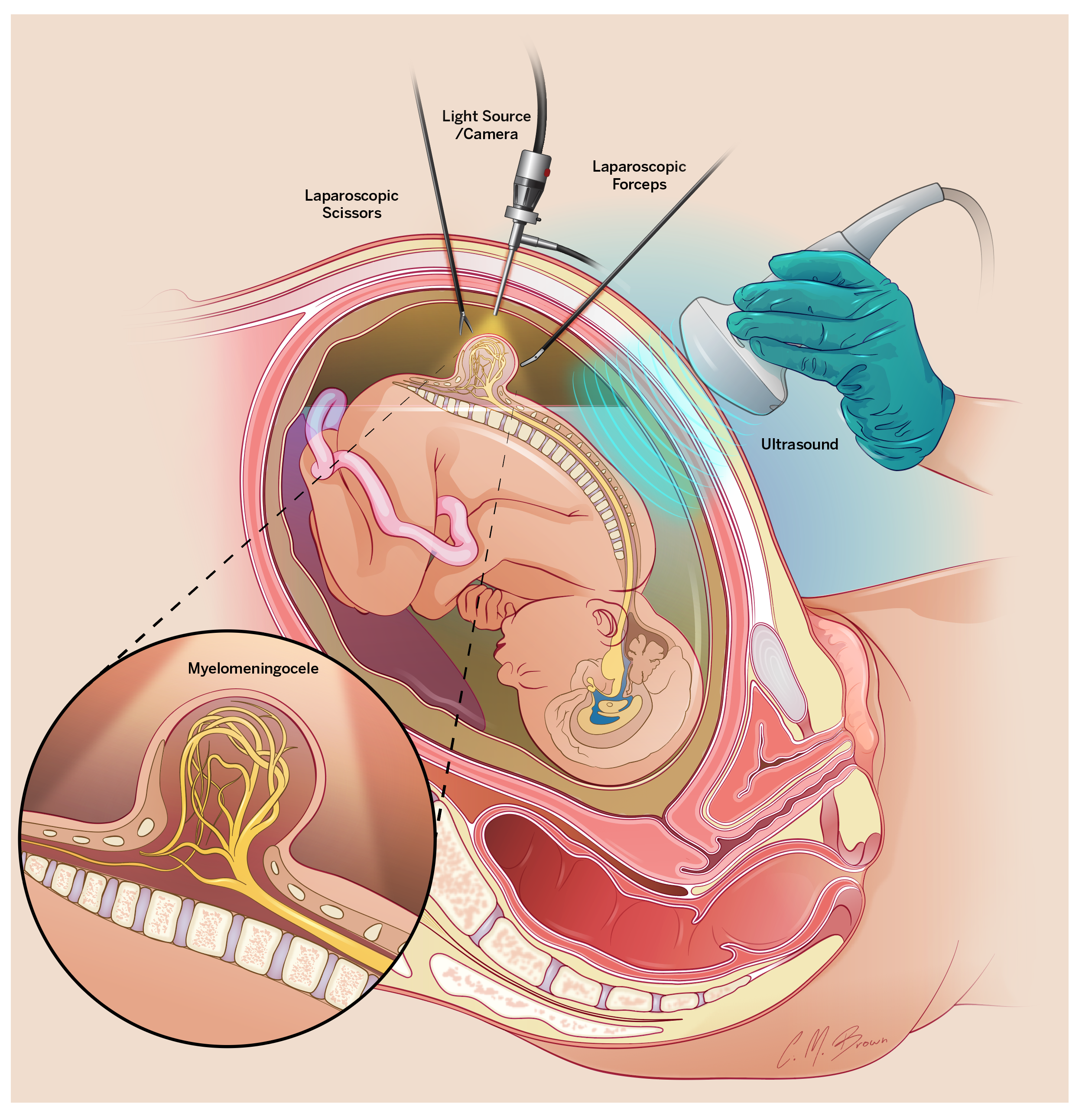
Myelomeningocele repair, also known as spina bifida or open neural tube defect repair, is a delicate fetal surgical procedure to close the neural placode in utero. Performed by fetal interventionalists and neurosurgeons, myelomeningocele repair is intended to prevent further damage to the baby’s spinal cord in the womb.
Benefits and risks of fetal myelomeningocele repair
The results of the Management of Myelomeningocele (MOMs) Trial suggest that fetal repair of myelomeningocele can have several beneficial effects for the baby. Fetal surgery for spina bifida can lead to a reduced risk of progressive damage to the spinal cord and nerves caused by exposure to amniotic fluid, improved mobility and walking as well as reduce the development of symptomatic hydrocephalus. With advancements in fetal surgery, especially procedures such as myelomeningocele repair, the life expectancy for children with spina bifida often extends into adulthood despite being a congenital condition.
Potential risks include preterm labor and preterm birth. Traditionally, the operation was completed through an “open approach.” This involved making a cesarean section-like skin incision to expose and open the uterus to operate on the baby’s back. This was found to increase the risk of maternal complications during the remainder of pregnancy, including uterine rupture, increased risk of wound infection and prolonged time to recovery. Additionally, the baby was required to be delivered via cesarean section.
Mini-laparotomy/Percutaneous Fetoscopic Myelomeningocele Repair
Given these maternal risks, our physicians were part of the pioneering team for a minimally invasive approach known as mini-laparotomy/percutaneous approach aimed at reducing the risk of large uterine incisions and achieving faster recovery for the mother, while maintaining the benefits to the baby.
The mother and fetus are eligible for surgery if:
- Mothers are at least 18 years old
- The fetus has a myelomeningocele lesion located between T1 and S1
- The fetus is between 19 and 26 weeks of gestation
- Mothers with a body mass index of less than 40 kg/m2
- Absence of uncontrolled maternal health conditions
- Absence of other associated severe fetal anomalies
- Normal fetal gestic testing confirmed via FISH, karyotype, or microarray
The mother is given general anesthesia and medication to prevent uterine contractions. The fetus also receives pain medication before the repair.
During the procedure, the fetal surgery team will perform a small skin incision on the mother’s abdomen and place three 4-millimeter ports into the uterus. These ports are used for the introduction of a small scope with a camera on the end (laparoscope) and surgical instruments into the womb to continue the operation on the baby. Some amniotic fluid is then removed and replaced with carbon dioxide gas to improve visualization.
The fetal surgery team then closes the spinal cord defect, protecting the fetal spinal cord and nerves from injury for the remainder of the pregnancy. The skin on the baby’s back is then closed to provide an additional layer of protection. The baby’s heart rate is checked frequently via ultrasound throughout the procedure.
Once the repair is complete, the amniotic fluid is replaced, and the ports are removed. The mother’s abdominal incision is then closed and gestation resumes.
What Happens After Fetal Surgery for Spina Bifida?
When the surgery is complete, the baby can continue growing and developing in the womb. Both mother and child will then remain in the hospital for a few days while recovering and monitoring the baby’s status. For the remainder of the pregnancy, the Fetal Center and the primary referring provider will monitor both mother and baby.
Our Spina Bifida Program will also provide ongoing care for your family. Our team of experts helps families prepare for the birth of a child with spina bifida and care for children into adulthood.
Key Points to Remember
Key Points to Remember
- Myelomeningocele (also referred to as an “open neural tube” defect) is the most severe form of spina bifida, where the spinal cord and nerves (also known as the “neural placode") develop on the outside of the body.
- The number and severity of problems in children with myelomeningocele varies depending on where the neural placode is located on the spine and how much of the spinal cord is affected.
- Myelomeningocele can be diagnosed early in pregnancy and most commonly during the anatomy ultrasound at routine prenatal visits and prenatal ultrasounds.
- Myelomeningocele repair, also known as spina bifida or open neural tube defect repair, is a delicate fetal surgical procedure to close the neural placode in utero.
FAQs
FAQs
What happens before the procedure?
- You will undergo detailed imaging: high-resolution ultrasound and fetal MRI.
- Amniocentesis is performed to collect amniotic fluid for genetic testing. This is done under ultrasound guidance using a fine needle.
- Lab work includes blood, urine, and vaginal cultures.
- Multidisciplinary consultations with your fetal surgeon, neurosurgeon, neonatologist, and others.
- A tour of the hospital and Spina Bifida Program may also be scheduled.
Will my insurance cover the procedure?
Once approved as a candidate, our team will seek prior authorization from your insurance provider. If denied, a physician may initiate a peer-to-peer review. Coverage decisions are case-specific, and our team works diligently to advocate for necessary care.
When will surgery be scheduled?
If you're eligible, surgery is scheduled between 24 and 26 weeks and 6 days of pregnancy.
What happens on the day of surgery?
- You will receive intravenous fluids and medications (indomethacin for uterine relaxation, Pepcid, Bicitra).
- You’ll meet with the surgical, anesthesia, and neurosurgery teams and sign surgery-related consents.
- Fetal monitoring
What should I expect during the surgery?
The procedure is performed under general anesthesia. You will be asleep during the surgery. Once you are under general anesthesia, a urinary catheter (Foley) will be inserted, and intravenous antibiotics will be administered to help prevent infection. An ultrasound will be performed to check several factors, including the baby’s head position and optimal locations for uterine entry. If the baby’s head is not facing downward, the team may perform an external cephalic version, a gentle maneuver on your abdomen, to turn the baby into a head-down position. Once this is complete and optimal positioning is confirmed, the fetoscopic spinal repair will begin.
How long does the surgery last?
You may be admitted the evening before or the morning of surgery. Admission time depends on final labs and evaluation completion.
We typically schedule surgery to begin at 8:00 AM. Initial steps include anesthesia administration and ultrasound assessment. If needed, the baby may be turned into a head-down position. The actual fetal repair generally begins between 10:30 and 11:00 AM and is expected to be completed by approximately 3:00 PM.
How will my pain be managed in the hospital and after discharge?
While still in the operating room, a member of the anesthesia team will mostly administer a spinal/epidural block before you receive general anesthesia. In addition, you will be offered an abdominal nerve block, which involves the injection of local anesthetic into the abdominal wall muscles using ultrasound guidance. This helps manage pain for the first 24 hours after surgery.
During your hospital stay, pain control will include a combination of medications such as acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs) if appropriate, and short-term use of opioids if necessary. Upon discharge, you will receive a personalized pain management plan that primarily includes acetaminophen, with a 2–3 day supply of opioid medication (such as oxycodone) if needed.
How long should I expect to stay in the hospital after surgery?
Patients are generally expected to stay for a minimum of three days following surgery (with surgery day counted as day zero). In some cases, a longer stay may be required to support recovery and ensure your safety.
How often will I be seen after surgery?
- You will have weekly ultrasounds to monitor your baby and uterus.
- Starting at 32 weeks, you will also have weekly non-stress tests (NSTs) to assess fetal well-being.
- At approximately 6 weeks post-surgery, we will conduct another fetal care conference with the above-mentioned teams, including an ultrasound and another MRI. Approximately 30% of fetuses may have reversal of hindbrain herniation after surgery, and the MRI will help identify this.
When will I likely deliver?
The average delivery timing is around 34–35 weeks. However, some patients deliver earlier, and others carry longer if stable. Your provider will monitor you closely and make recommendations based on your and your baby’s health.
What happens after birth?
Your baby will be cared for in the NICU and evaluated by neurosurgery and other specialists. Additional support, such as physical therapy, urology, and developmental care, may begin shortly after birth.
The average NICU stay for babies with spina bifida is about two to four weeks, but this can vary from a few days to several months depending on the specifics of the baby’s medical condition and the gestational age at delivery. The earlier the gestational age at delivery, the longer the stay.
Will my baby need other future surgeries or procedures?
Yes, your baby may need additional surgeries or procedures in the future. These can include surgeries to manage hydrocephalus, surgery to manage tethered cord in which the spinal cord is stuck or pulled tight instead of moving freely, orthopedic procedures to address mobility issues, and interventions for bowel and bladder dysfunction.
Support Services & Resources
Support Services & Resources
We offer a broad range of supportive services to make life better for families who choose us for their children's care.
Spina Bifida research, education, support, clinical care, network building and advocacy
The Hydrocephalus Association (HA) is the nation’s largest and most widely respected organization dedicated to hydrocephalus.
Related Stories
Related Stories

Meet the Riley neurosurgeons providing nationally ranked care with broad subspecialty expertise
At Riley Children’s Health, highly skilled pediatric neurosurgeons manage complex brain, spine and nervous system conditions in children of all ages, from infants to young adults.
Continue reading
How we’re redefining the standard for children with spina bifida
Pediatric urologists at Riley Children's Health are nationally acclaimed for improving the standard of care for children with spina bifida.
Continue reading
