
Riley Children’s Health is now among a select group of institutions nationwide, and only at this time in the Midwest, to offer a novel, minimally invasive surgical technique for myelomeningocele. Mini-laparotomy/percutaneous fetoscopic repair of open spina bifida is an innovative approach that minimizes the risk of fetal surgery for the mother, while preserving the benefits of in-utero repair for the fetus.
This groundbreaking procedure is the result of a unique collaboration between maternal fetal medicine and pediatric neurosurgery in the Fetal Center at Riley Children’s Health. The first surgery in Indiana was performed in February by Dr. Hiba Mustafa, director of Fetal Surgery and Dr. Jason Chu, pediatric neurosurgeon, alongside a team of specialists including neonatology, radiology, and others.
“Since the MOMS trial, prenatal repair of myelomeningocele has focused on minimizing manipulation of the uterus,” said Dr. Chu. “A large incision in the maternal abdomen and then another to expose the uterus—and the ensuing uterine manipulation—are what we believe lead to complications for the mother, such as uterine rupture, placental abruption and spontaneous labor.”
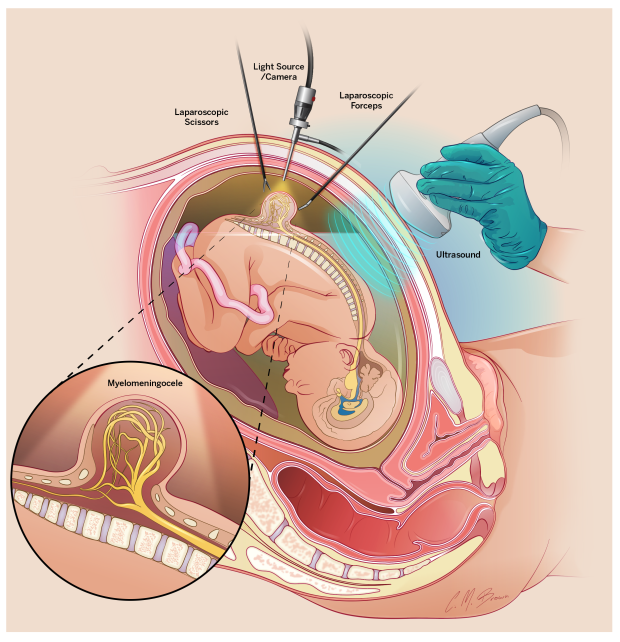
An alternative to the traditional “open approach” of prenatal myelomeningocele repair, the mini-laparotomy requires a skin incision of just 2 to 3 centimeters. Through this incision in the mother’s abdomen, the fetal surgery team places three ports into the uterus. The ports are used to introduce the fetoscope and surgical instruments into the womb to close the spinal cord defect. “There’s very little manipulation of the uterus, which reduces the risk for maternal complications,” Dr. Chu said.
“It’s been our experience so far that mothers also recover faster compared to the traditional open procedure, with an increased potential for the babies to be born closer to term, as well as for vaginal delivery—an outcome that isn’t possible when the uterus has been exposed as part of the procedure.”
For the fetus, mini-laparotomy fetoscopy decreases the risk of hydrocephalus, improves hindbrain herniation and results in improved developmental and motor outcomes in patients with open neural tube defects.
"We’re excited to offer this minimally invasive surgical procedure to patients in Indiana and the Midwest," says Dr. Chu. "Our expert team provides complete care—before and after the surgery, with the comprehensive Spina Bifida Program at Riley Children’s delivering additional care and support after the babies are born. To see a successful outcome and follow these babies as they grow up is incredibly rewarding. It’s a testament to the collaboration and dedication of our entire team."




